Results of DA VINCI, an EU Wide Cross-Sectional Observational Study of Lipid-Modifying Therapy Use in Secondary and Primary Care, underline the need for combination therapy for patients at highest risk and in whom the lowest LDL-C goals are recommended.
DA VINCI study: Change in approach to cholesterol management will be needed to reduce the implementation gap between guidelines and clinical practice in Europe.
What guidelines recommend and the clinical reality for lipid management in routine practice differ. This issue was previously highlighted by the EUROASPIRE (European Action on Secondary and Primary Prevention by Intervention to Reduce Events) study in secondary prevention patients. This survey showed that 71% of these very high-risk patients had low-density lipoprotein cholesterol (LDL-C) values below the European Society of Cardiology/European Atherosclerosis Society (ESC/EAS) guideline goals set in 2016 (1,2). Lack of awareness of guideline recommendations was a potential factor contributing to suboptimal lipid management (1).
In 2019, the ESC/EAS updated guidelines for lipid management (3). This revision took account of evidence that lowering LDL-C levels below the 2016 ESC/EAS goals improves clinical benefit, based on landmark studies with ezetimibe (IMPROVE-IT) (4) and PCSK9 monoclonal antibody therapy (FOURIER and ODYSSEY OUTCOMES) (5,6). Consequently, LDL-C goals were lowered for moderate to very high cardiovascular risk patients. Additionally, in high and very high-risk categories, at least 50% reduction in LDL-C levels from baseline, a proxy for the use of high-intensity of statin, was also added (Table 1).
Table 1. ESC/EAS guideline recommended LDL-C goals

Importantly, the 2019 ESC/EAS guidelines also recognised the high and very high-risk of certain primary prevention patient groups, including those with diabetes or familial hypercholesterolaemia (FH) without established atherosclerotic cardiovascular disease (ASCVD), or with chronic kidney disease (3). While statins are first line treatment to lower LDL C, the guidelines also recommended combination with non-statin LDL-lowering therapy to achieve the stringent new targets.
One year on, it is important to review how these revised guidelines might be implemented in routine practice. This was the aim of the DA VINCI study (EU Wide Cross-Sectional Observational Study of Lipid-Modifying Therapy Use in Secondary and Primary Care) (7).
DA VINCI included 5,888 patients (3,000 primary prevention patients and 2,888 secondary prevention patients) from 18 European countries. Patients aged ≥18 years who were prescribed lipid lowering therapy (LLT) at or within 12 months of enrolment, and had an LDL-C measurement up to 14 months before enrolment, attended for measurement of LDL-C. The primary outcome was the proportion of patients on stabilised LLT (i.e. no change in dose or regimen for at least 28 days before the LDL-C assessment visit) who achieved their risk-based LDL-C goal. Cardiovascular risk was based on SCORE (Systematic Coronary Risk Evaluation) and estimated glomerular filtration rate for primary prevention patients, and REACH for patients with established ASCVD. While the primary outcome related to the 2016 ESC/EAS guideline goals, a post hoc analysis also evaluated goal attainment based on the 2019 ESC/EAS guidelines.
In comparison to prior studies one quarter of patients were enrolled from primary care sites. Of the secondary prevention patients, almost all (97%) had ASCVD, either cerebrovascular disease (41%), peripheral artery disease (37%) or coronary disease (22%). This provides new information in two groups of patients at high risk previously understudied namely (peripheral arterial disease and cerebrovascular disease). ASCVD patients tended to be older (mean age 68 versus 63 years) with a lower proportion of female patients (34% versus 50%) compared with the primary prevention group. The very high-risk of ASCVD patients was exemplified by REACH cardiovascular risk predictions; 82% had a 10-year risk of a cardiovascular event >20% and 31% had a 10-year risk >40% despite use of lipid lowering therapies. By contrast, most (67%) primary prevention patients were at low to moderate risk, with only 4% categorised as very high-risk based on SCORE.
Lipid lowering therapy and goal attainment
Stabilised LLT at the LDL-C assessment visit was predominantly statin (94% of patients), with moderate intensity statin most commonly prescribed in both groups. High-intensity statin monotherapy was prescribed in 38% of ASCVD patients (versus 22% of primary prevention patients). Overall statin monotherapy was the predominant mode of lipid lowering therapy used (84%). There was limited use of combination therapy: 9% of patients received ezetimibe with moderate or high intensity statin, and 1% of patients received a PCSK9 inhibitor combined with a statin and/or ezetimibe.
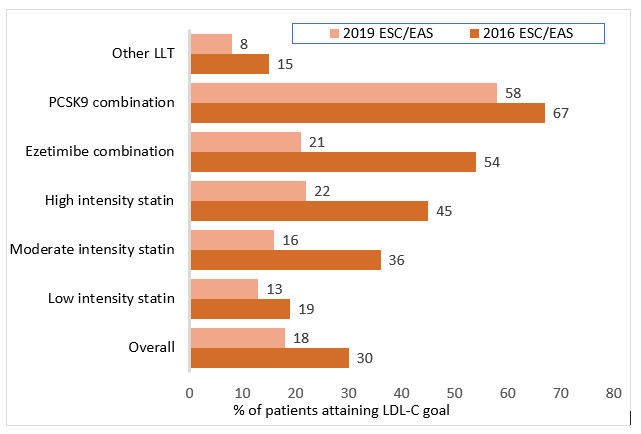
Goal achievement was suboptimal. Overall, only about half (54%) of the patients attained their 2016 ESC/EAS guideline risk-based goal, and this was even lower (33%) for 2019 ESC/EAS guideline goals. Among patients with ASCVD, goal achievement was even lower; whereas 30% had LDL-C levels <1.8 mmol/L only 18% – less than one in five – achieved LDL-C levels <1.4 mmol/L. When assessing 2016 ESC/EAS goal attainment (LDL-C < 1.8mmol/L), this increased as expected from use of low to high intensity statins (19-45%), and further with combination therapy (54% with ezetimibe and 67% with PCSK9 inhibitors). When the goal became harder to reach i.e. <1.4mmol/L (ESC/EAS 2019 goal), then every regimen including combination therapy with ezetimibe resulted in about one fifth goal attainment. By contrast, for patients on PCSK9 inhibitor combination 58% had levels <1.4 mmol/L (Figure 1). Importantly, even when statin monotherapy was optimised, LDL-C levels remained above 2.0 mmol/L.
Among primary prevention patients, differences in LDL-C goal attainment were less dramatic. For example, in moderate-risk primary prevention patients (the predominant group), LDL-C levels <3.0 mmol/L were achieved by 81% and levels <2.6 mmol/L by 66% on moderate intensity statin monotherapy, the most commonly prescribed regimen. For very high-risk primary prevention patients goal attainment remained low.
Figure 1. LDL-C goal attainment in ASCVD patients: 2016 ESC/EAS versus 2019 ESC/EAS guideline goals
What have we learned from the DA VINCI study?
The resounding message from the DA VINCI study is that clinicians need to change their thinking with respect to how they manage high and very high-risk patients in routine practice. This challenge was already evident from studies which assessed LDL-C goal attainment based on the 2016 ESC/EAS guidelines (1,8). With even more stringent LDL-C goals introduced by the 2019 ESC/EAS guidelines, goal attainment is even lower. Failure to optimise the use of high-intensity statin therapy is one factor. It is, however, clear that the 2019 ESC/EAS LDL-C goal for high and very high-risk patients is largely unattainable on high-intensity statin monotherapy; such patients also require combination therapy. A practical message from DA VINCI is to assess risk and if the LDL-C goal is <1.8 mmol/L, consider early use of combination therapy with ezetimibe as suggested by the 2019 ESC/EAS algorithm. However, the DA VINCI study demonstrates that for very high-risk patients, around four in five will likely require PCSK9 inhibitor combination therapy, potentially without the ezetimibe step.
Although efficacious, the use of adjunctive PCSK9 monoclonal antibody therapy in routine practice has practical issues, such as cost and local reimbursement difficulties. Clinicians may also have concerns regarding the safety of very low LDL-C levels attained on this treatment. Clearly, there are opportunities for further education, about safety, efficacy, and the unmet clinical need.
Finally, why is it so important to attain these guideline-recommended LDL-C goals, particularly in ASCVD patients? These patients are at high residual risk of cardiovascular events. For example, using the SMART (Second Manifestations of Arterial Disease) risk score, a quarter of acute coronary syndrome patients have a 10-year risk of recurrent events exceeding 20%, even with optimal risk factor management (9). In the DA VINCI study, this residual risk was even higher; about one in three ASCVD patients had a 10-year risk of cardiovascular events exceeding 40%. LDL-C is a major contributor to this residual risk, and thus guideline-recommended LDL-C management should be prioritised.
DA VINCI has clearly highlighted opportunities to optimise LDL-C management in routine practice. To achieve this, educational programmes are essential, supported by academic societies such as the EAS. Improving the translation of the 2019 ESC/EAS guideline recommendations for lipid management to clinical practice is critical to reducing the high residual cardiovascular risk in ASCVD patients. In Europe where there are approximately 22 million patients with ASCVD, extrapolating the DA VINCI data to Europe suggests as many as 18 million will not reach the ESC/EAS 2019 LDL-C goals, unless steps are taken to consider combination therapy for those at highest risk and in whom the lowest LDL-C goals are recommended. The lipid field needs to recognise the lessons of the hypertension field where combination therapy has become the norm.
References
1. De Backer G, Jankowski P, Kotseva K, et al. Management of dyslipidaemia in patients with coronary heart disease: Results from the ESC-EORP EUROASPIRE V survey in 27 countries. Atherosclerosis 2019;285:135-46.
2. Catapano AL, Graham I, De Backer G, et al. 2016 ESC/EAS guidelines for the management of dyslipidaemias. Eur Heart J 2016;37:2999-3058.
3. Mach F, Baigent C, Catapano AL, et al. 2019 ESC/EAS Guidelines for the management of dyslipidaemias: lipid modification to reduce cardiovascular risk. Eur Heart J 2020;41:111-88.
4. Giugliano RP, Cannon CP, Blazing MA, et al. Benefit of adding ezetimibe to statin therapy on cardiovascular outcomes and safety in patients with versus without diabetes mellitus: Results from IMPROVE-IT (Improved Reduction of Outcomes: Vytorin Efficacy International Trial). Circulation 2018;137:1571-82.
5. Sabatine MS, Giugliano RP, Keech AC, et al. Evolocumab and clinical outcomes in patients with cardiovascular disease. N Engl J Med 2017;76:1713-22.
6. Schwartz GG, Steg PG, Szarek M, et al. Alirocumab and cardiovascular outcomes after acute coronary syndrome. N Engl J Med 2018;379:2097-107.
7. Ray KK, Molemans B, Schoonen WM et al. EU-Wide Cross-Sectional Observational Study of Lipid-Modifying Therapy Use in Secondary and Primary Care: the DAVINCI study. Eur J Prev Cardiol 2020:doi:10.1093/eurjpc/zwaa047
8. Kotseva K, De Backer G, De Bacquer D, et al. Primary prevention efforts are poorly developed in people at high cardiovascular risk: A report from the European Society of Cardiology EURObservational Research Programme EUROASPIRE V survey in 16 European countries. Eur J Prev Cardiol 2020:2047487320908698. doi: 10.1177/2047487320908698.
9. Zafeiropoulos S, Farmakis I, Kartas A, et al. Risk for recurrent cardiovascular events and expected risk reduction with optimal treatment 1 Year after an acute coronary syndrome. Am J Cardiol 2020:S0002-9149(20)30780-3.