Atherosclerosis newsletter
Highlighted articles from January issue Vol 388
Newsletter by Editor in Chief Prof Arnold von Eckardstein, and Editorial Office Manager Simona Negrini
Join the Atherosclerosis social media community on Facebook (Atherosclerosis – Journal of the European Atherosclerosis Society) and Twitter (@ATHjournal) for scientific discussion and information about the journal.
Socioeconomic status, environment, and lifestyle behavior are well known factors that have considerable impact on the risk and outcome of atherosclerotic cardiovascular diseases. They have direct and indirect effects on the pathogenesis of atherosclerosis and they frequently confound other risk factors and pathologies. The present issue has several articles reporting on the interactions of social, environmental and lifestyle factors with measurable risk factors in the prediction and management of cardiovascular risk.
Social disadvantage, coronary artery calcium, and their interplay in the prediction of atherosclerotic cardiovascular disease events
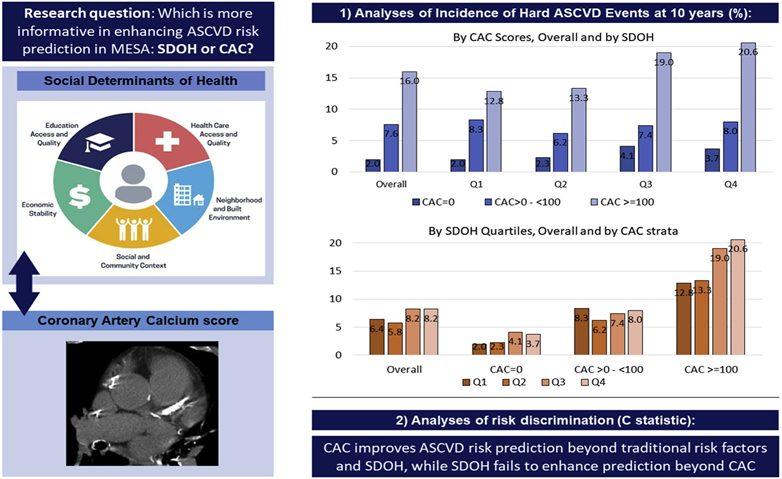
There is increasing recognition of social determinants of health (SDOH) as upstream determinants of life expectancy and multiple acute and chronic conditions, including atherosclerotic cardiovascular disease (ASCVD). This makes SDOH highly informative in the identification of populations and groups at increased risk of developing ASCVD who may benefit from targeted public health, policy, and other population-level preventive interventions. However, whether at the individual level SDOH improve current ASCVD risk prediction paradigms beyond traditional risk factors and the coronary artery calcium (CAC) score is unknown. Acquah et al. evaluated the interplay between CAC and SDOH in ASCVD risk prediction.
Multi-Ethnic Study of Atherosclerosis (MESA) participants (6479) who had baseline information on all relevant SDOH variables and CAC score data were included in this analysis. An SDOH index inclusive of 14 items from 5 domains (economic stability, neighborhood and physical environment, education, community and social context, and healthcare access and quality) was used. The index range was 0–1 and was divided into quartiles, with higher ones representing worse SDOH. Cox regression was used to evaluate the adjusted associations between CAC, SDOH, their interplay, and ASCVD events. The C-statistic was computed to assess improvement in risk discrimination for prediction of ASCVD events.
ASCVD incidence increased with increasing CAC scores across SDOH quartiles. The lowest incidence was observed in those with CAC = 0 and favourable SDOH (2/1000 person-years) and the highest in those with CAC>100 and most unfavourable SDOH (20.6/1000 person-years). While CAC was strongly associated with ASCVD across SDOH quartiles, SDOH was weakly associated with ASCVD across CAC strata. CAC improved the discriminatory ability of all prediction models beyond traditional risk factors. Improvements with SDOH were smaller, and were none on top of CAC.
CAC improves ASCVD risk stratification across the spectrum of social vulnerability, while SDOH fail to improve risk prediction beyond traditional RFs and CAC.
In their editorial, Kadiyala et al. discuss these findings in more details.
Assessment of ethnic inequalities in diagnostic coding of familial hypercholesterolaemia (FH): A cross-sectional database study in Lambeth, South London
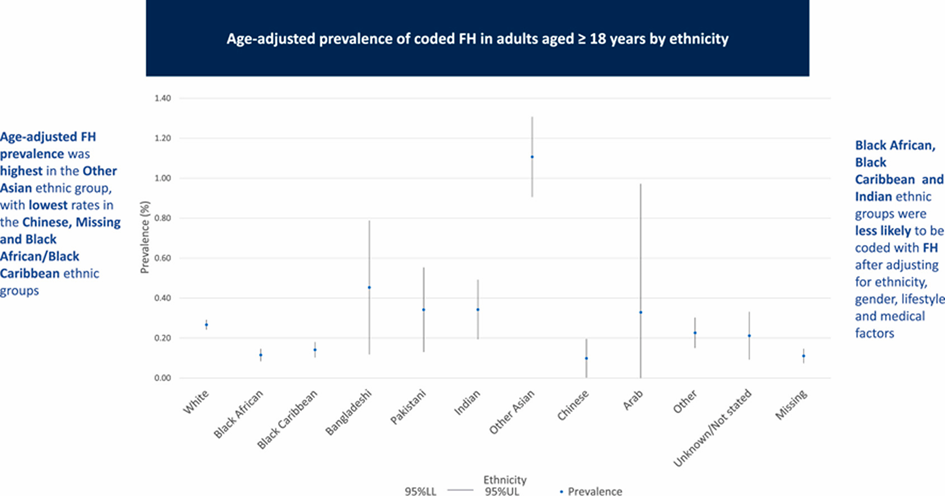
Familial hypercholesterolemia (FH) is associated with high levels of low-density lipoprotein cholesterol disease (LDL-C) leading to development of cardiovascular CVD at younger ages, with highest relative risk at age <40 years. Differences in the perceived prevalence of familial hypercholesterolemia (FH) by ethnicity are unclear. In this study, Molokhia et al. aimed to assess the prevalence, determinants and management of diagnostically-coded FH in an ethnically diverse population in South London.
A cross-sectional analysis of 40 practices in 332,357 adult patients in Lambeth was undertaken. Factors affecting a (clinically coded) diagnosis of FH were investigated by multi-level logistic regression adjusted for socio-demographic and lifestyle factors, co-morbidities, and medications.
The age-adjusted FH % prevalence rate ranged from 0.10 to 1.11. Lower rates of FH coding were associated with age and male gender. Compared to a White British reference group, a higher likelihood of coded FH was observed in Other Asians, with lower rates in Black Africans, Indians, and in Black Caribbeans. The overall prevalence using Simon Broome criteria was 0.1%.
Lower likelihoods of FH coding were seen in non-native English speakers, most deprived income quintile, smokers, hypertension, chronic kidney disease, obesity, diabetes and CVD. 20% of FH coded patients were not prescribed lipid-lowering medications.
Inequalities in diagnostic coding of FH patients exist. Lower likelihoods of diagnosed FH were seen in Black African, Black Caribbean and Indian ethnic groups, in contrast to higher diagnoses in White and Other Asian ethnic groups. Hypercholesterolaemia requiring statin therapy was associated with FH diagnosis, however, the presence of cardiovascular disease (CVD) risk factors lowered the diagnosis rate for FH.
Parental cardiovascular disease and cardiovascular disease risk factors in the offspring: The Diet, Cancer and Health cohorts
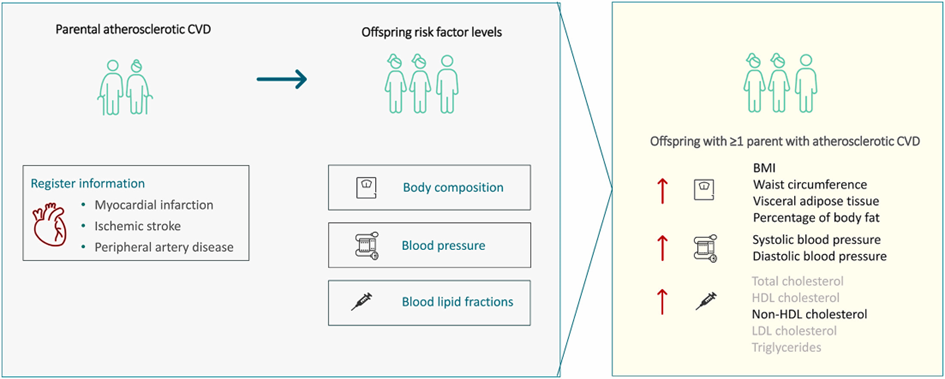
Cardiovascular disease (CVD) aggregates in families and offspring with parental CVD may have adverse risk factor levels long time before the potential onset of CVD. Petersen et al. compared risk factor levels in offspring of parents with atherosclerotic CVD (ASCVD) and parents with no ASCVD at different parental ages at onset.
The study included 5751 participants of the Diet, Cancer and Health – Next Generations study. Measurements included blood pressure, body composition and lipid fractions. Information on parental ASCVD and age at disease onset was obtained through register linkage. Parental ASCVD was defined as myocardial infarction, ischemic stroke or peripheral artery disease occurring <70 years, prematurely, divided into age categories or using a broader classification of CVD. Linear regression models using generalized estimating equations were used for analysis. Analyses were adjusted for age, sex, education, smoking, alcohol intake, physical activity and some additionally for BMI.
Offspring with parental ASCVD had a higher blood pressure, waist circumference, BMI, visceral adipose tissue, percentage of body fat and non-HDL cholesterol levels, but not other lipid levels, compared to offspring with no parental ASCVD. Overall, the same patterns were observed for parental ASCVD occurring prematurely and using a broader CVD classification.
Findings were overall consistent across different classifications of parental ASCVD.
Association between long-term exposure to ambient air pollution and lesion ischemia in patients with atherosclerosis
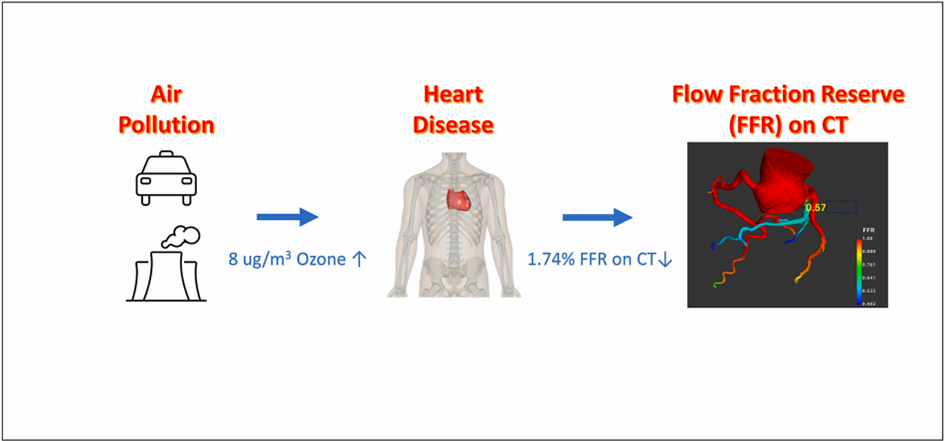
Coronary heart disease (CHD) is the leading cause of death worldwide. Air pollution is an emerging factor in determining the risk of adverse coronary events. Evidence from meta-analyses and large-scale cohort studies has shown that long-term exposures to ambient air pollutants is associated with an increased risk of cardiovascular disease morbidity and mortality. However, few studies have focused on the underlying mechanistic pathways. Xu et al. aimed to fill the gaps in physiological mechanisms between air pollution and CHD by examining the associations of long-term exposure to ambient air pollutants with functional coronary stenosis and lesion ischemia assessed by novel fractional flow reserve on computed tomography (CT-FFR).
CT-FFR, which defines a ratio of maximal myocardial blood flow compared to its normal value, was characterized in 2017 patients with atherosclerosis between 2015 and 2017. Exposure to ozone (O3), nitrogen dioxide (NO2), and fine particulate matter (PM2.5) was estimated using high-resolution exposure models. Linear and logistic regression models were used to assess the association of each air pollutant with CT-FFR and with the prevalence of clinically relevant myocardial ischemia (CT-FFR <75%).
Participants were on average 60.1 years old. Annual mean O3, NO2, PM2.5 were 61, 47 and 60 μg/m3, respectively. Mean CT-FFR value was 76.9%. In the main analysis, a higher level of O3 was associated with a lower CT-FFR value and a higher prevalence of myocardial ischemia, adjusting for potential confounders such as risk factors and plaque phenotypes, independent of the effects of exposure to NO2 and PM2.5. No associations were observed for PM2.5 or NO2 with CT-FFR. Long-term exposure to O3 is associated with lower CT-FFR value in atherosclerotic patients, indicating higher risk of lesion ischemia.
Interactive effects of physical activity and sarcopenia on incident ischemic heart disease: Results from a nation-wide cohort study
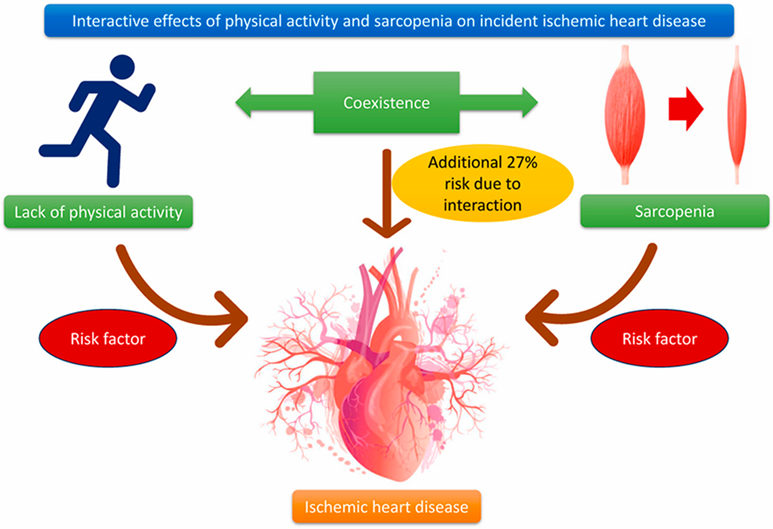
Cardiovascular diseases (CVDs) are the leading causes of death worldwide. Ischemic heart disease (IHD), accounts for about 50% of all cardiovascular deaths. Physical activity (PA) is a health-relevant lifestyle factor, which is generally considered to have various benefits on both physical and mental health. Strong evidence supports that PA is one of the modifiable risk factors tightly associated with CVD outcomes. Sarcopenia is a disease characterized by progressive and generalized loss of skeletal muscle mass and strength. Growing evidence suggests that sarcopenia is strongly associated with various adverse health outcomes, including falls, frailty, mortality, and several measures of age-related functional decline. Lack of PA and sarcopenia are known risk factors for IHD. However, considering their coexistence in the middle-aged and elderly population, the interaction of these two factors remains uncertain. Here, Lai et al. investigated the interactive effects of PA and sarcopenia on IHD.
Data on 344,688 participants free of IHD at baseline were extracted from the UK Biobank. PA was classified into low, moderate, and high according to the International Physical Activity Questionnaire. Sarcopenia was identified in accordance with the European Working Group on Sarcopenia in Older People 2. Cox proportional hazard models were applied to estimate the effect of PA and sarcopenia on incident IHD and its subtypes. Objective PA data measured by wrist-worn devices were used to repeat the analyses.
Over a median follow-up of 11.7 years, 24,809 (7.2%) participants developed incident IHD. Lack of PA was associated with a higher risk of IHD after adjusting for potential confounders. The hazard ratio (HR) was 1.09 (95% CI: 1.05–1.13) for individuals without sarcopenia and 1.29 (95% CI: 1.17–1.42) for those with sarcopenia. Regarding the joint effect, the combination of low PA and sarcopenia was associated with the highest risk of IHD, and both additive and multiplicative interactions were significant. For subtypes of IHD, the interaction was pronounced in acute myocardial infarction and chronic ischemic heart disease. These results suggest a synergistic interaction between lack of PA and sarcopenia on the risk of IHD. Findings from this study may help facilitate more effective primary prevention of IHD.
Timing of clinic visits after health checks and risk of hospitalization for cardiovascular events and all-cause death among the high-risk population
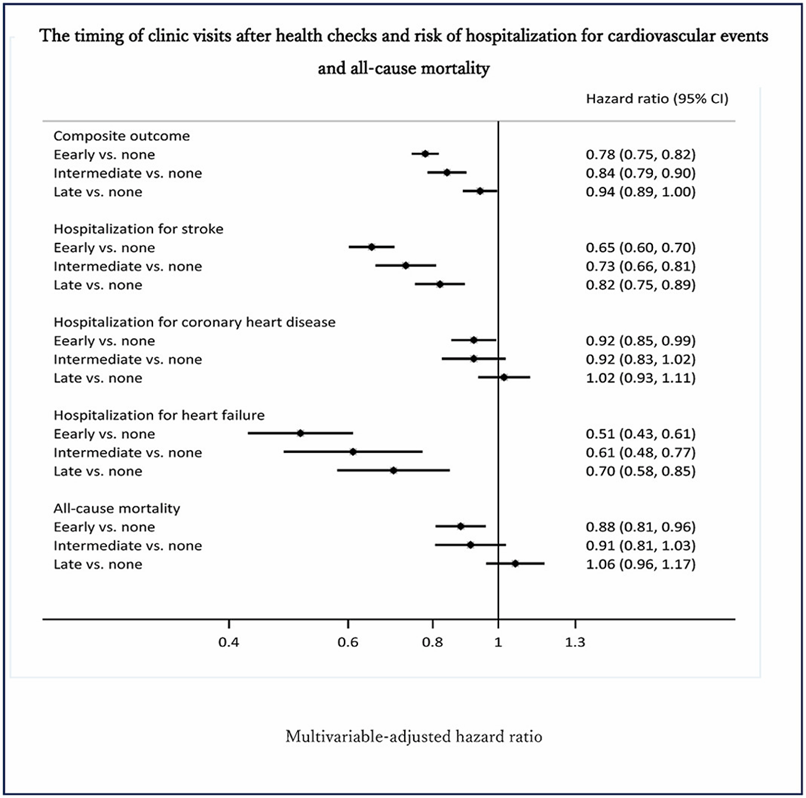
Health checks have been long considered effective in the primary prevention of chronic diseases; a number of observational studies provided evidence that people with frequent health checks experienced a lower risk of mortality and delays in medical care seeking by clinic visits could therefore reduce the beneficial effect of health checks. Current evidence is lacking in supporting an effective role of health checks in CVD prevention. Dong et al. aimed to examine the association between timing of clinic visits after health checks and risk of hospitalization for cardiovascular events and all-cause mortality among the high-risk population.
A total of 412,059 high-risk individuals from the health claims database of the Japan Health Insurance Association were divided into 4 groups according to the timing of clinic visits during 12 months after health checks. Cox proportional hazard regression models were used to examine the associations between timing of clinic visits after health checks and risk of hospitalization for stroke, coronary heart disease, heart failure, or all-cause mortality.
During a median follow-up of 4.3 years, a total of 15,860 cases having composite outcomes of first hospitalization for stroke, coronary heart disease, heart failure, or all-cause mortality were identified. Compared to high-risk adults without clinic visits after the health checks, the fully adjusted hazard ratios of a composite outcome were 0.78, 0.84, and 0.94 for early, intermediate, and late clinic visits, respectively. Compared to no clinic visit, an early clinic visit was associated with lower risks of all individual endpoints, and the risk reductions appeared to be greater in the hospitalization for stroke and heart failure. The results suggest that that an early clinic visit after health checks was associated with lower risks of hospitalization for major cardiovascular events and all-cause mortality among high-risk individuals.