Debunking the myth: familial hypercholesterolaemia does not protect against diabetes
The FHSC Investigators, led by the FHSC Coordinating Centre at Imperial College London, present an article titled Association of BMI, lipid-lowering medication, and age with prevalence of type 2 diabetes in adults with heterozygous familial hypercholesterolaemia: a worldwide cross-sectional study that was published this month in Lancet Diabetes and Endocrinology.
Familial hypercholesterolaemia (FH), a genetic defect in cholesterol uptake, leads to a deficiency in LDL receptors, limiting cholesterol uptake in tissues like the pancreas, which was thought to prevent pancreatic lipotoxicity — a contributing factor to diabetes. And a relatively low diabetes prevalence has been reported in some FH cohorts.
However, this global study of approximately 24,000 adults with FH found a diabetes prevalence of 5.7%, closely aligning with general population rates reported by the Global Burden of Disease (6.1%) and International Diabetes Federation (4.6%). Further, most world regions had a higher diabetes prevalence than Europe (Figure 1). These findings challenge the idea that FH protects against diabetes, and suggest that the low diabetes rates reported in Western FH cohorts may largely reflect careful lifestyle management.
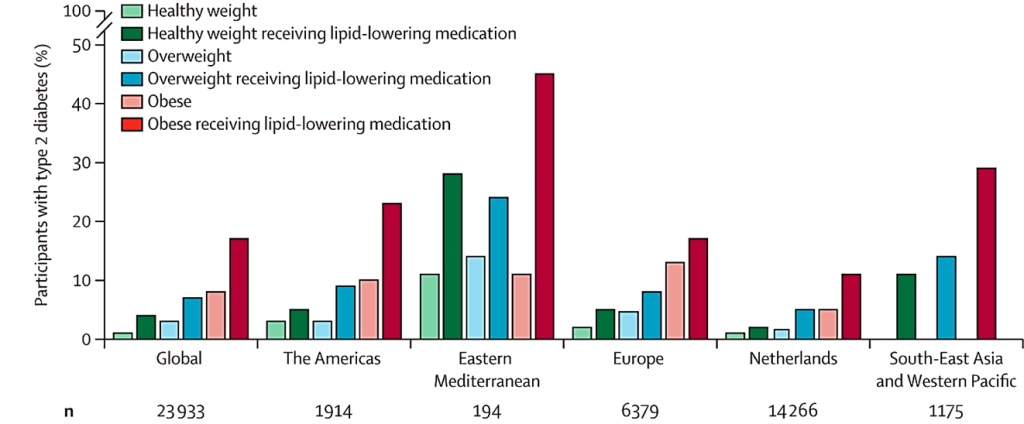
Figure 1. Prevalence of diabetes in patients with FH globally and by world region, stratified by weight categories and receipt of lipid-lowering medication (including statins).
The research also indicates that, while statins — the standard lipid-lowering medication in FH — are linked to higher probability of diabetes, the absolute risk of developing diabetes is greater in those with obesity, at all ages, and independent of medication (Figure 2).
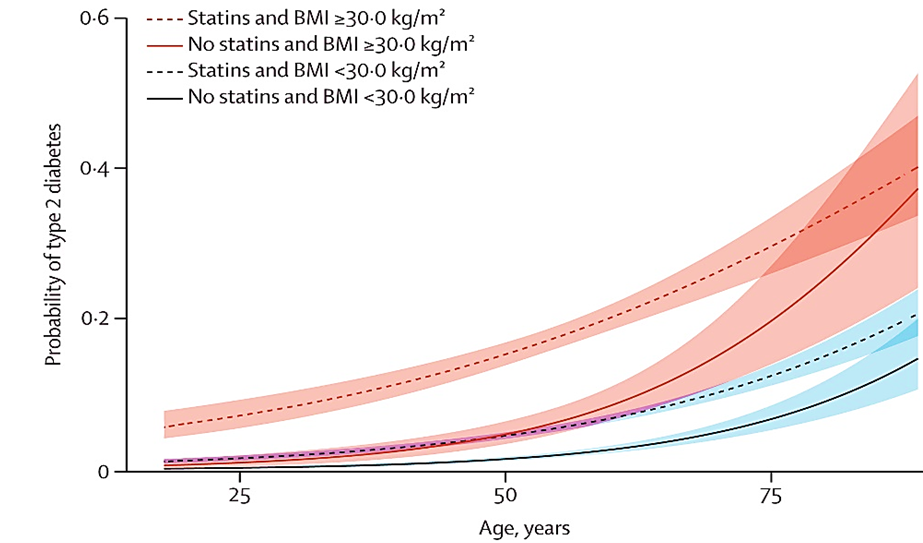
Figure 2. Predicted probability of having type 2 diabetes patients with FH as a function of age, presence of obesity (BMI≥30 kg/m2) and use of statins, adjusted for sex.
Given that advancing age and statin therapy are common factors contributing to diabetes risk in patients with FH, addressing obesity as a key modifiable risk factor is crucial for reducing diabetes risk in these patients.