Atherosclerosis newsletter
Highlighted articles from August issue Vol 395
Newsletter by Editor in Chief Prof Arnold von Eckardstein, and Editorial Office Manager Simona Negrini
Join the Atherosclerosis social media community on Facebook (Atherosclerosis – Journal of the European Atherosclerosis Society) and Twitter (@ATHjournal) for scientific discussion and information about the journal.
It is increasingly recognized that life style and environmental factors play an important role in the pathogenesis of atherosclerosis by modulating classical risk factors such as dyslipidemia and hypertension and independently thereof. The August volume of Atherosclerosis contains several articles addressing these aspects.
Lifestyle factors as determinants of atherosclerotic cardiovascular health
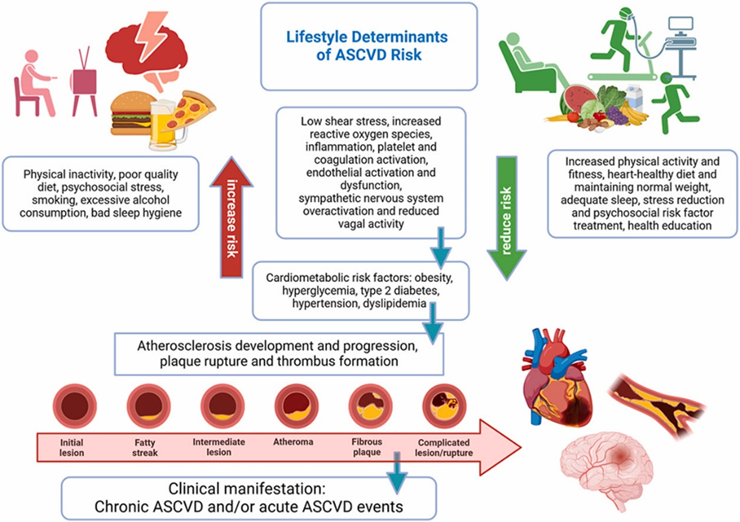
A sedentary lifestyle, low levels of physical activity and fitness, poor dietary patterns, and psychosocial stress are associated with increased morbidity and mortality from atherosclerotic cardiovascular disease (ASCVD). Conversely, regular physical activity, healthy dietary patterns, and psychosocial stress-reduction are important determinants of atherosclerotic cardiovascular disease (ASCVD) health.
In this review, Schmidt-Trucksäss et al. summarize current evidence from large observational studies and randomized controlled trials on lifestyle factors as determinants of ASCVD health. Moreover, they describe mechanistic insights into how factors such as low shear stress, increased reactive oxygen species production, chronic inflammation, platelets and coagulation activation, endothelial dysfunction, and sympathetic hyperactivity contribute to the initiation and exacerbation of ASCVD risk. Practical recommendations to facilitate the translation of scientific knowledge into interventions to promote ASCVD health are outlined.
Women’s reproductive risk score and healthy lifestyle modification in cardiovascular disease: Findings from the UK Biobank
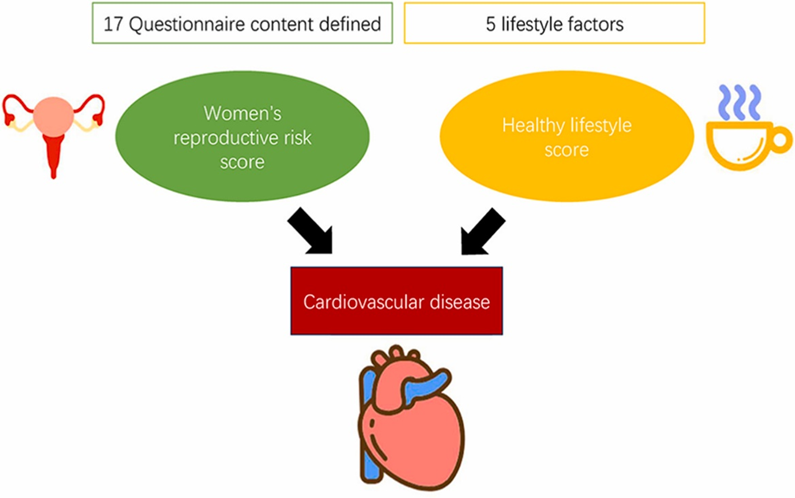
Underdiagnosis of CVD in women suggests that extra efforts are needed to focus on this specific population. The latest clinical guidelines also call for increased sensitivity in detection of CVD among young women. Reproductive risk factors are associated with increased risk of cardiovascular disease (CVD) in women. However, the combined effects of the composite reproductive risk factors on CVD are unknown. Huang et al. aimed to construct a reproductive risk score (RRS) to measure reproductive status, examine the association between RRS and CVD, and explore the modification effect of healthy lifestyle on the association in women in the UK Biobank cohort.
The RRS was constructed for 74,141 female participants with data from the UK Biobank and was derived from 17 baseline variables, all of which indicative of women’s reproductive health status. Four categories of RRS status were defined: low-risk group (score 0–1); low-intermediate group (score 2–3); high-intermediate group (score 4–5); and high-risk group (score 6–13). A healthy lifestyle score (HLS) with five related factors was also constructed, and the following categories were defined: unhealthy lifestyle group (score: 0–1), intermediate lifestyle group (score: 2–3) and healthy lifestyle group (score: 4–5).
Each point increase in RRS was associated with a 22 % higher risk of CVD, 23 % higher risk of ischemic heart disease (IHD) and 19 % higher risk of stroke. The percentage population-attribution risks (PAR%) were 16 % for CVD, 15 % for IHD and 18 % for stroke. A healthy lifestyle significantly attenuated RRS associations with the incidence of CVD and IHD. The attributable proportions due to additive interaction between RRS and HLS were 0.14 for CVD and 0.15 for IHD, respectively.
In summary, high RRS was associated with increased risks of CVD, IHD and stroke in female participants in the UK Biobank. Early-stage identification of women with reproductive risk using synthesised indicators and healthy lifestyle interventions could be useful for the prevention of CVD.
The Nutri-Score nutrition label: Associations between the underlying nutritional profile of
foods and lipoprotein particle subclass profiles in adults
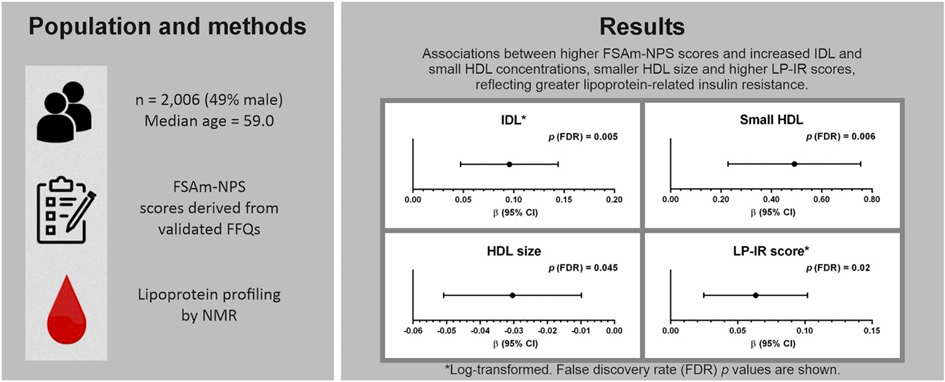
The association between diet and chronic conditions is thought to be due to complex interactions between foods and nutrients; studies have therefore highlighted the importance of characterising diet-cardiometabolic health relationships through assessment of dietary patterns and dietary indices. Lipoprotein particle concentrations and size are associated with increased risk for atherosclerosis and premature cardiovascular disease. Certain dietary behaviours may be cardioprotective and public health strategies are needed to guide consumers’ dietary choices and help prevent diet-related disease. The Food Standards Agency nutrient profiling system (FSAm-NPS) constitutes the basis of the five-colour front-of-pack Nutri-Score labelling system. No study has examined FSAm-NPS index associations with a wide range of lipoprotein particle subclasses. Millar et al. aimed to assess the relationship between the FSAm-NPS scoring system and plasma lipid and lipoprotein profiles, including lipoprotein particle concentrations and sizes, to test the hypothesis that poorer nutritional quality according to Nutri-Score rating would be associated with a less favourable lipoprotein subclass metabolic profile.
This cross-sectional study included 2006 middle-to older-aged men and women randomly selected from a large primary care centre. Individual participant FSAm-NPS dietary scores were derived from validated food frequency questionnaires. Lipoprotein particle subclass concentrations and size were determined using nuclear magnetic resonance spectroscopy. Multivariate-adjusted linear regression analyses were performed to examine FSAm-NPS relationships with lipoprotein particle subclasses.
In fully adjusted models, which accounted for multiple testing, higher FSAm-NPS scores, indicating poorer dietary quality, were positively associated with intermediate-density lipoprotein and small high-density lipoprotein (HDL) concentrations, a lipoprotein insulin resistance score, reflecting greater lipoprotein-related insulin resistance, and inversely associated with HDL size.
Consuming foods with a poorer Nutri-Score rating is associated with a less favourable lipoprotein particle subclass profile. A less pro-atherogenic lipoprotein status may be a potential mechanism underlying reported health benefits of a healthy diet according to Nutri-Score rating.
See the editorial by Haslam and Mora to gain more insights into the results of this the cross-sectional study.
Dietary n-3 alpha-linolenic and n-6 linoleic acids modestly lower serum lipoprotein(a) concentration but differentially influence other atherogenic lipoprotein traits: A randomized
trial
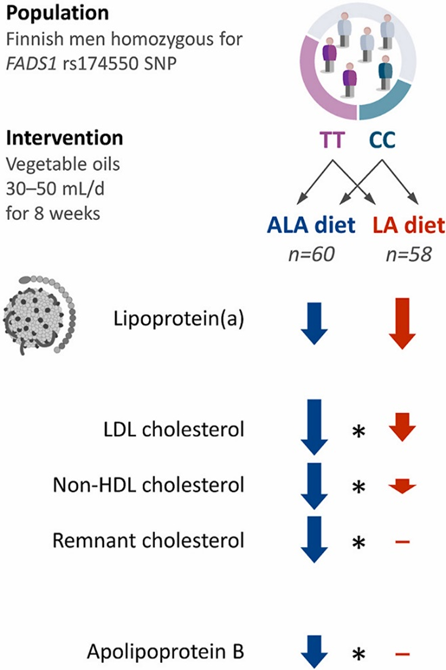
Elevated lipoprotein(a) [Lp(a)] is a well-established causal risk factor for cardiovascular diseases (CVD). Although plasma concentration of Lp(a) is predominantly determined by genetics, up to 10–30 % of variability in Lp(a) concentrations can be attributed to lifestyle. Indeed, some lifestyle factors, including diet, have been reported to modulate serum Lp(a) concentrations. Limited evidence suggests that dietary unsaturated fat may increase serum Lp(a) concentration by 10–15 %. Linoleic acid (LA) may increase Lp(a) concentration through its endogenous conversion to arachidonic acid, a process regulated by the fatty acid desaturase (FADS) gene cluster. Nuotio et al. aimed to compare Lp(a) and other lipoprotein trait-modulating effects of dietary alpha-linolenic (ALA) and LA. Additionally, they examined whether fatty acid desaturase 1 (FADS1) rs174550 genotype modifies Lp(a) responses.
A genotype-based randomized trial was performed in 118 men homozygous for FADS1 rs174550 SNP (TT or CC). After a 4-week run-in period, participants were randomized to 8-week intervention diets enriched with either Camelina sativa oil (ALA diet) or sunflower oil (LA diet) 30–50 mL/day based on their body mass index (BMI). Serum lipid profile was measured at baseline and at the end of the intervention.
ALA diet lowered serum Lp(a) concentration by 7.3 % and LA diet by 9.5 %. Both diets led to a greater absolute decrease in individuals with higher baseline Lp(a) concentration. Concentrations of LDL cholesterol (LDL-C), non-HDL-C, remnant-C, and apolipoprotein B were more decreased by the ALA diet. FADS1 rs174550 genotype did not modulate diet-induced changes in Lp(a) concentration or other lipoprotein traits.
A considerable increase in either dietary ALA or LA from vegetable oils has a similar Lp(a)-lowering effect, whereas ALA may lower other major atherogenic lipids and lipoproteins to a greater extent than LA. The use of poly-unsaturated fatty acids (PUFAs) for the prevention of CVD is also discussed in the editorial by Lehnert et al.
Low-level ambient ozone exposure associated with neutrophil extracellular traps and pro-atherothrombotic biomarkers in healthy adults
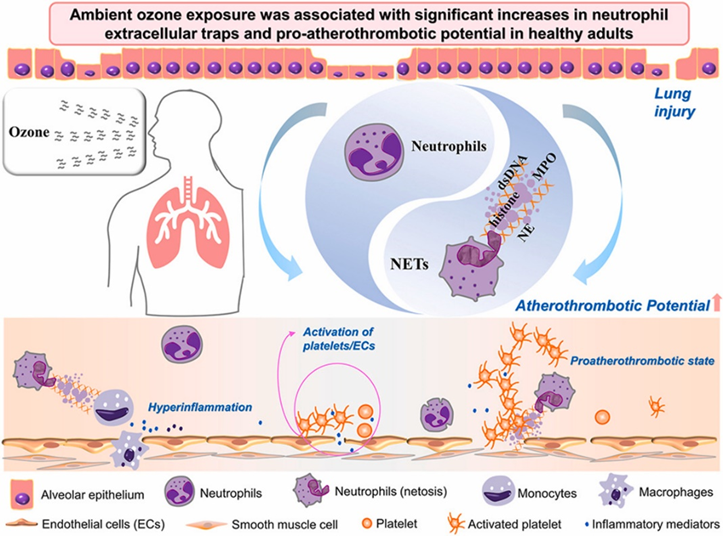
Global levels of ambient ozone (O3) exposure have been reported to exceed the air quality guidelines (AQGs) of the World Health Organization (WHO) across various regions, such as South and East Asia. Emerging studies have indicated that ambient O3 exposure may prompt cardiovascular diseases (CVDs), however, the observational associations were less convincing and could be confounded by co-pollutants. The recent Ozone Integrated Science Assessment has shown that the current evidence is suggestive but insufficient to conclude a causal association between ambient O3 exposure and CVD mortality, in part because the cardiovascular pathophysiologic changes responsive to O3 have not been clearly observed in humans. Xu et al. aimed to examine the pro-atherothrombotic impacts of O3 exposure and to explore the potential mediating roles of dysfunctional neutrophils, focusing on neutrophil extracellular traps (NETs).
A longitudinal panel study of 152 healthy adults was conducted in the cool to cold months, with relatively low levels of O3, between September 2019 and January 2020 in Beijing, China. Four repeated measurements of indicators reflecting atherothrombotic balance and NETs were performed for each participant.
Daily average exposure levels of ambient O3 were 16.6 μg/m3 throughout the study period. Per interquartile range increase in average concentrations of O3 exposure at prior up to 7 days, an increase of 200.1–276.3% in D-dimer, 27.2–36.8% in thrombin-antithrombin complex, 10.8–60.3% in plasminogen activator inhibitor 1, 13.9–21.8% in soluble P-selectin, 16.5–45.1% in matrix metalloproteinase-8, and 2.4–12.4% in lipoprotein-associated phospholipase A2 was observed. These pro-atherothrombotic changes were accompanied by endothelial activation, lung injury, and immune inflammation. O3 exposure was also positively associated with circulating NETs indicators, including citrullinated histone H3, neutrophil elastase, myeloperoxidase, and double-stranded DNA. Mediation analyses indicated that NETs could mediate O3-associated pro-atherothrombotic responses. The observational associations remained significant and robust after controlling for other pollutants, and were generally greater in participants with low levels of physical activity.
Ambient O3 exposure was associated with significant increases in NETs and pro-atherothrombotic potential, even at exposure levels well below current air quality guidelines of the World Health Organization.
These results are further discussed in Artner and Lang editorial.