EAS is pleased to announce that Professor Helen Hobbs, Dallas, USA will be the recipient of the Anitschkow Prize 2019. This prestigious Prize, awarded annually by EAS, recognizes outstanding research in the field of atherosclerosis and linked metabolic disturbances. The 2019 award recognizes the critical role that Professor Hobbs has played in defining the genetic determinants of plasma lipid levels and cardiovascular risk.
Professor Hobbs has made outstanding contributions from both clinical, genetic and basic science areas to understanding of cholesterol metabolism, atherosclerosis and regulation of energy metabolism.
About the Winner
Helen H. Hobbs, M.D., is an Investigator of the Howard Hughes Medical Institute and a Professor of Internal Medicine and Molecular Genetics at the University of Texas Southwestern Medical Center. She holds the Dallas Heart Ball Chair in Cardiology Research, the Philip O’Bryan Montgomery Jr., M.D., Distinguished Chair in Developmental Biology, and the Eugene McDermott Distinguished Chair for the Study of Human Growth and Development. She obtained her undergraduate degree from Stanford University prior to attending Case Western Reserve University School of Medicine.
After completing an internship in internal medicine at Columbia-Presbyterian Medical Center, she moved to Dallas, Texas where she finished her clinical training and served as chief resident in internal medicine at Parkland Memorial Hospital. She worked as a postdoctoral fellow in the laboratory of Drs. Michael Brown and Joseph Goldstein before joining the faculty of UT Southwestern in 1987.
Currently, Professor Hobbs is Director of the McDermott Center for Human Growth and Development, which serves as the Center for Human Genetics at UT Southwestern. She is also Director of the Dallas Heart Study, a longitudinal, multiethnic, population-based study of Dallas County. Her professional affiliations include the Arteriosclerosis, Thrombosis and Vascular Disease Council of the American Heart Association, the Association of American Physicians, the American Society of Human Genetics and the American Society of Clinical Investigation. Professor Hobbs has received numerous awards, most recently the Passano Award (with Jonathan Cohen) in 2016, and the Breakthrough Prize in Life Sciences and Pearl Meister Greengard Prize, Rockefeller University, both in 2015.
The research
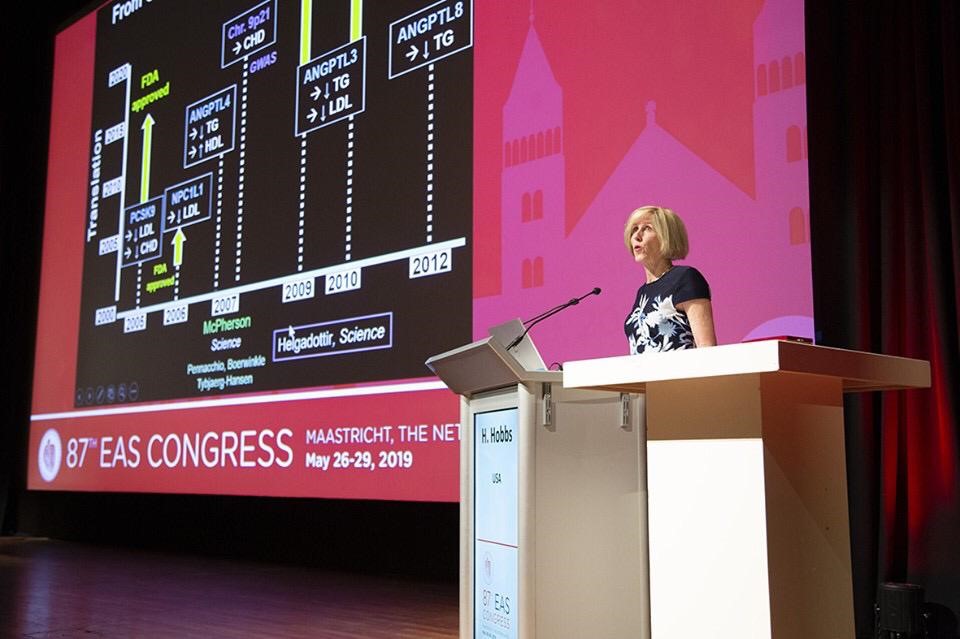
Professor Hobbs’s research focuses on defining the genetic determinants of plasma lipid levels and cardiovascular risk. In her early work she investigated the culprit gene (LDLRAP1) that is inactivated in autosomal recessive hypercholesterolaemia, as well as defective variants in ABCG5 and ABCG8 which play a role in sitosterolaemia. In the design of the Dallas Heart Study, she joined forces with Jonathan C. Cohen to focus on rare and low-frequency genetic variants that contribute to complex diseases, such as coronary atherosclerosis. Together, they hypothesized that if low-frequency variants with large effects were present in the population, their identification would expedite the translation of a genetic association into a therapeutic product. This ‘sequencing the extremes” strategy was critical to the discovery of loss-of-function mutations in PCSK9 that were associated with low plasma LDL-C levels and protection from atherosclerotic cardiovascular disease, and subsequent development of novel PCSK9-targeted therapeutics.
In later research she identified genetic variations that confer susceptibility to fatty liver disease. In genome-wide association studies, Professor Hobbs identified a single nucleotide polymorphism in patatin-like phospholipase domain–containing protein 3 (PNPLA3), which is associated with an increase in hepatic triglyceride content, as the most important genetic risk factor for fatty liver disease. The effect of this variant is substantially amplified by obesity and insulin resistance. A second risk allele for hepatic steatosis was identified in a gene that encodes transmembrane 6 superfamily member 2 (TM6SF2). Subsequent research has shown that both variants are associated with the full spectrum of alcoholic as well as non-alcoholic fatty liver disease, albeit via different mechanisms. More recently, her research has identified a loss-of-function variant of hydroxysteroid 17-β dehydrogenase that is associated with a reduced risk of chronic liver disease and reduced progression of fatty liver disease. Akin to the PCSK9 story, these findings provide a rationale for a new therapeutic approach for this increasingly common disease.